
Overactive bladder – maybe you’ve heard the term before, but what does it mean?
Overactive bladder (OAB) is characterized by a cluster of symptoms including:
- Increased voiding frequency
- Urgency (with or without leaking)
- Nocturia (waking up to urinate at least 2 times per night).
According to the National Association for Continence, OAB affects approximately 33 million women in the US, and many of these women also reported issues of incontinence.
So what’s the big deal?
Well, when you are always worried about locating the nearest bathroom, it begins to shape your choices and affect your day-to-day activities.
This is not simply a physical condition that causes inconvenience – it profoundly affects emotional and mental health as well. It can disrupt your sex life and dramatically affect your sleep.
Embarrassment and shame can seriously diminish your quality of life. When incontinence is present, there is often a fear of leaking and of not knowing if you will “make it” to a bathroom in time.
As I hinted above, women who report symptoms of OAB often demonstrate significantly higher levels of stress and anxiety (Knight et al, 2013).

Likewise, studies have shown that mindfulness and meditation can be helpful in reducing symptoms. Both of these practices help us to “downtrain” our nervous system, helping us slow down, breathe, and be present in the moment.
It is very important to note that an Overactive Bladder is NOT just a normal occurrence due to age or after having a baby!
It is also important to distinguish the difference between common and normal.
Frequent voiding, pain in your pelvis or abdomen, and leaking of any amount are NOT NORMAL, despite the fact that so many women are dealing with these symptoms!
How do you know if you have an Overactive Bladder?
OAB is diagnosed based on history and physical examination and is NOT considered a disease, but rather a cluster of symptoms. Your physician will perform a physical exam and may order testing such as urinalysis to rule out underlying conditions or infection.
The following criteria are present in Overactive Bladder:
- Voiding more than 8 times per day
- Getting up to void more than once per night
- Urinary urgency
- Urgency incontinence (not necessary for diagnosis, but often present)
Now for the Good News – OAB Can Be Successfully Treated!
OAB responds very well to a holistic treatment approach that includes pelvic floor therapy, behavioral therapy (bladder training), along with lifestyle changes including nutritional and stress management.
The American Urological Association recently released guidelines for the treatment of OAB (Lightner et al, 2019).
Behavioral therapy, bladder retraining, and pelvic floor muscle training are listed as first-line treatments! In other words, due to evidence supporting these interventions, they should be your first resort, not a last-ditch effort!
The guidelines encourage seeking conservative care first while avoiding surgical and pharmacological management to achieve the best outcomes (Lightner et al, 2019).
Behavioral Therapy and Bladder Training
Behavioral therapy and bladder training begin with the use of a Bladder Diary, which keeps track of fluid intake, voiding patterns, leaking, and urging intensity.
It also includes information that can help identify possible behavioral bladder triggers such as turning a key in a door or turning on the water for a shower.

A Pelvic Floor Therapist can help you analyze these results and come up with a treatment plan.
When you understand more about how your bladder should operate, it gives you perspective and the empowerment to know things can be different.
For more information on how a “happy bladder” functions, check out the previous post about normal bladder function (Read More).
Urge Suppression Techniques
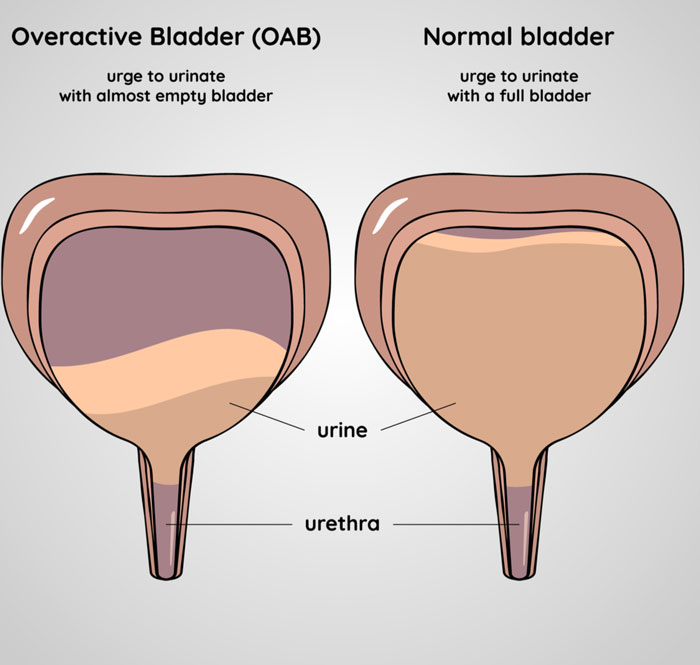
With OAB, you feel a strong urge to urinate despite your bladder not actually being full.
Learning urge suppression and distraction techniques along with addressing fluid intake can help decrease the frequent trips to the bathroom and help with the uncomfortable urges.
Over time, the bladder learns to fill completely and you gain control over when you decide to go.
Reducing bathroom trips by 50% can be life-changing for someone who is going 15-20 times in one day! And that’s totally achievable for many women!
Distraction techniques may include things like mental math, making lists in your head, crossword puzzles, wiggling toes, foot and ankle exercises, deep breathing, and meditation. Many women are surprised by the power of distraction!

Increasing Voiding Intervals
Bladder training will also include a systematic increase in voiding intervals.
For example, if your diary shows that you are voiding every hour, you may begin with a goal of every 1.5 hours, employing the strategies mentioned above, and working your way up from there as instructed by your pelvic floor therapist.
Nutrition and Diet
Foods that decrease urinary pH and make the urine more acidic may lead to inflammation or irritation in the bladder lining, causing increased urgency.
Foods containing Arylalkylamine may also lead to irritation. A few of the more common potential bladder irritants include:
- Alcohol
- Citrus
- Caffeine
- Coffee
- Carbonated beverages

I know! I know! It’s all of the good stuff!
I am not saying that everyone has to give up their coffee, or their cocktails, but it is absolutely worth investigating.
Using an elimination diet can identify your “top offenders”, and then you can decide if it is worth it to you to cut them out of your daily routine.
You may find that just decreasing the frequency or amount of one of these can make a big difference.
I often work with women who have decreased their water intake with the hope of urinating less, but, ironically, this actually leads to MORE frequent voiding due to highly concentrated urine.
A good rule of thumb is to drink approximately half your body weight in water (in fluid ounces) each day.
What do we do with all of this information?
The information gathered from your diary along with the physical evaluation can help you and your Pelvic Floor Therapist put together a plan of action to help get to the root of the issue.
In the case of leaking, or Urge Incontinence (Read More), pelvic floor therapy will identify and address weakness, tightness, and pain in the pelvic floor.
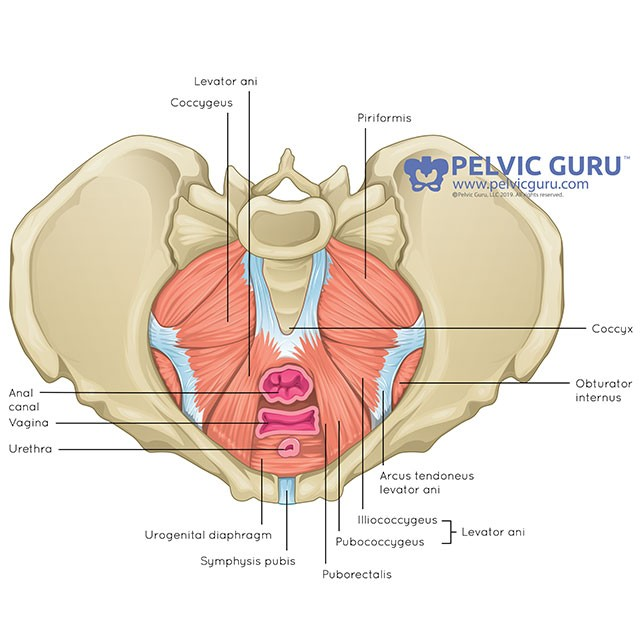
Your pelvic floor is a group of muscles that runs from your pubic bone to your tailbone and supports your pelvic organs like a hammock or sling.
These muscles are important for bowel and bladder control, sexual health, and stabilizing your hips and pelvis.
For more information on the pelvic floor, check out this previous blog post which goes into great detail (Read More).
Hypertonicity (chronic muscle tension) of the pelvic floor muscles often mimics urges and feels like bladder pain.
These feelings of urgency or bladder pain lead to an increased frequency of voiding.
Inappropriate abdominal contraction such as “over-gripping” your abdominals or habitually “sucking in your belly” can also lead to increased urgency.
Increased muscle tension over time leads to shortening, making it difficult for these muscles to fully lengthen and perform the role they were designed to perform.
How do we address tightness?
One of the ways a Pelvic Floor Therapist treats tightness or hypertonicity is with “manual therapy,” which includes a variety of hands-on techniques such as myofascial release, trigger point therapy, and strain/counter strain.
These techniques aren’t just focused on the pelvic floor, as we must address the areas surrounding the pelvis such as the abdomen and hips.

Restrictions in these adjacent regions can significantly contribute to OAB symptoms.
Manual techniques are incredibly important as they restore the muscles’ ability to lengthen.
However, you also need to be able to ACTIVELY engage and relax your pelvic floor in everyday life.
One of the best ways to achieve this is by learning how to connect your breath to your pelvic floor.
I wrote extensively about the role that breathing plays in the pelvic floor – check out this blog post to Read More.
Hypertonicity is also associated with an “upregulated” Sympathetic Nervous System, in which you are spending the majority of your time in a “fight, flight or freeze” state. Your brain and body are constantly on guard, leading to increased nerve activity and muscle tone.
Learning how to downregulate your nervous system is an acquired skill.
Numerous research studies support the idea that you can decrease your stress response by practicing daily meditation, mindfulness, and deep breathing.

Combining these practices with “pelvic floor opening” and restorative yoga poses can also be helpful in reducing tone in the pelvic floor.
So There Is Hope After All!
Overactive Bladder is often multifactorial, and thus, so is the appropriate treatment.
Addressing issues within the pelvic floor, as well as dietary changes, stress management, and behavior changes are all important components of a successful treatment program.
If you’re wondering if you’re dealing with an Overactive Bladder, but you don’t know where to start, fill out the contact form to request more information on how pelvic floor therapy can help!



