Prostate cancer may seem like a somber subject, but it is extremely important to discuss, particularly in the context of pelvic health physical therapy. Prostate cancer is the second most commonly diagnosed cancer in American males, and it is one of the most common reasons why a male would need to work with a pelvic health physical therapist. Let’s start with some important background information.
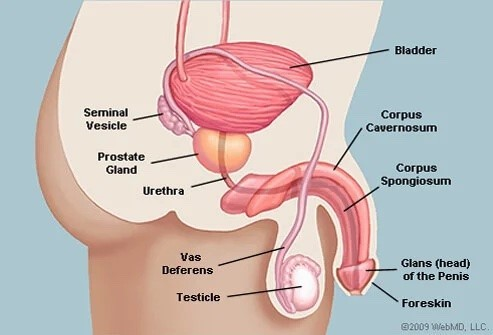
What is the prostate?
The prostate is a small gland located directly beneath the bladder and in front of the rectum. Normally, it is about the size of a walnut and contains a portion of the urethra (the urinary tract that carries urine out of the penis), allowing urine to pass through and exit the body. The prostate naturally grows as men age. This is not problematic UNLESS it obstructs urine flow (called benign prostatic hyperplasia or BPH) or if growth of those cells is unchecked and results in cancer.
Who tends to develop prostate cancer?
All males have a small risk for developing prostate cancer simply because they have a prostate. Age, ethnicity, and genetic risk factors contribute to increased risk for some men. As men age, the risk of developing prostate cancer increases because cells continue to grow in the prostate. African American and Caucasian males have the highest risk for developing prostate cancer based on ethnicity. Family history can also indicate risk for developing prostate cancer, including:
- First-degree male relative (father, brother, son) on either mother or father’s side of the family with prostate cancer
- First-degree female relative (mother, sister, daughter) diagnosed with breast, ovarian, or pancreatic cancer
- Relative diagnosed with prostate cancer at age 55 or younger
What are the symptoms of prostate cancer?
Symptoms for prostate cancer can vary widely. Some men do not even show symptoms! Common symptoms can include:
- Difficulty initiating urine flow
- Weak or slow urine stream
- Incomplete bladder emptying
- Frequent urination
- Blood in urine or semen
- Painful ejaculation
- Pain in low back, hips, and/or pelvis that doesn’t go away and/or isn’t affected by movement
How is prostate cancer diagnosed?
The most common method for determining the presence of prostate cancer is a Prostate Specific Antigen (PSA) test. PSA is made by the prostate and can be found in the blood. If levels of PSA are above a certain value, a person is more likely to have prostate cancer.
Many things can affect PSA levels, such as age, ethnicity, and inflammation or injury. To figure out if cancer is causing higher PSA levels, a biopsy is performed. Once the biopsy has been performed, tests are run on the tissue to see if cancer is present. If cancer is present, a Gleason Score is assigned based on the likelihood of the cancer to spread. A lower Gleason Score indicates a lower likelihood that cancer will spread.
Finally, the cancer will be staged, or categorized, based on the amount of tissue involved and where that tissue is located. For example, if the cancer has remained in the prostate, it is classified as being non-aggressive. This type of cancer is staged with a lower number. If the cancer has spread (metastasized) to other areas, either local to the prostate (lymph nodes) or further away (bones), this type of cancer is classified as being aggressive. More aggressive cancer is staged with a higher number.
What are the treatment options for prostate cancer?
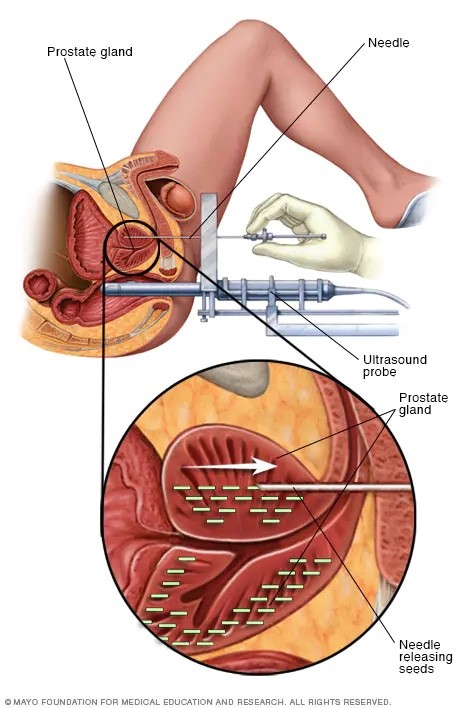
Once prostate cancer has been diagnosed and staged, there are several different treatment options. If the cancer is not aggressive, the medical team may opt for active surveillance or “watchful waiting.” This means they will monitor PSA levels at regular intervals and adjust the treatment plan if levels change dramatically.. Radical prostatectomy, or surgical removal of the prostate, is another option in which surgeons try to remove all the cancerous tissue. Radiation therapy is another common form of treatment for prostate cancer. External radiation therapy utilizes a machine to direct beams of very high energy into the tissues to kill the cancerous cells. Internal radiation therapy (brachytherapy) involves surgical implantation of radioactive seeds or pellets into the prostate to destroy cancer cells. Other forms of treatment for prostate cancer include chemotherapy, cryotherapy, hormone therapy, biological therapy, and high-intensity focused ultrasound.
Treatment for prostate cancer can bring about many additional challenges for men as they learn how to navigate in their “new” physical state. Depending on the type of treatment chosen, men can experience varying degrees of urinary incontinence, urinary urgency/frequency, pelvic and/or abdominal pain, impotence, decreased muscle mass/strength, and loss of muscle or tissue flexibility.
How can pelvic floor physical therapy help patients with prostate cancer?
Pelvic health physical therapy can help men as they navigate and manage a prostate cancer diagnosis by addressing all of the side effects of treatment listed above. Ideally, men should see a pelvic health physical therapist immediately after a diagnosis of prostate cancer and before cancer treatment to learn about:
- Appropriate function of pelvic floor muscles
- Pelvic floor anatomy and how it will change after a prostatectomy
- Diaphragmatic breathing and nervous system regulation
- Erectile dysfunction due to prostatectomy and ways to address this
- Scar and fascial mobilization
- Strengthening activities to ensure pelvic floor muscles and overall strength are maximized, particularly if additional treatment is necessary
- Maximizing quality of life and urinary/sexual function
After treatment, it is extremely important to return to pelvic health physical therapy to address changes in muscle and tissue that can cause incontinence, pain, tissue restriction due to scarring, and/or muscle weakness. A physical therapist can teach exercises and movement strategies to prevent incontinence, which is a common side effect after prostate cancer treatment. Patients also learn how to stretch or mobilize tissue that may be affected by surgical or radiation scars, regulate their nervous system post-treatment, and work on general strengthening and returning to previous daily and recreational activities. Pelvic health physical therapy is a constructive outlet for patients faced with a diagnosis of prostate cancer.
If you or someone you know is managing a prostate cancer diagnosis, please contact us at Limitless Therapy and Wellness. We are here, ready to jump in with tools and skills to navigate the physical part of this cancer journey as well as walk alongside you with emotional support.
Sources:
Centers for Disease Control and Prevention. 2021. Prostate Cancer. [online] Available at: Prostate Cancer | CDC [Accessed 9 June 2022].